If you’ve been diagnosed with a varicocele, you may have more choices for treatment than you realise. One advanced option is varicocele embolization, a minimally invasive, non-surgical procedure that serves as an alternative to traditional surgery. It has helped thousands of men successfully treat varicoceles, often allowing them to return to normal activities within just a few days. Many men opt for this non-surgical option since it avoids general anaesthesia, scrotal cuts, and stitches.
What Is a Varicocele ?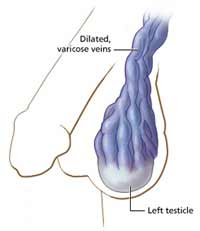
Varicocele is a relatively common condition (affecting approximately 10 percent of men) that tends to occur in young men, usually during the second or third decade of life. At times, varicoceles don’t produce any symptoms and remain harmless. But sometimes a varicocele causes pain or atrophy (shrinkage) of testis, or fertility problems.
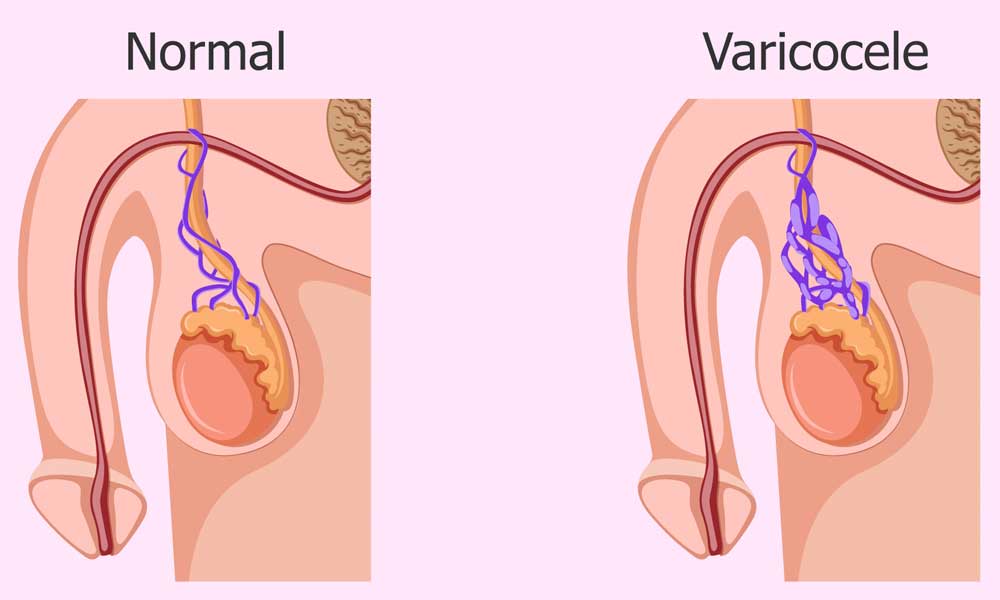
Typically, blood reaches the testicles through an artery and drains away through a network of small veins that connect to a larger vein running up through the abdomen. Blood in this vein is meant to move upward toward the heart, with one-way valves ensuring it doesn’t flow backward into the testicles.
What Causes Varicoceles?
These one-way valves sometimes fail. The reverse flow of blood stretches and enlarges the tiny veins around the testicle to cause a varicocele, a tangled network of blood vessels, or varicose veins (see Figure above)
Varicocele Symptoms
Most varicocele symptoms are mild and often don’t need treatment. However, if the condition leads to pain or any of the issues mentioned below, treatment may be recommended.
Signs & symptoms of Varicoceles
Pain
A common indication of varicoceles is a dull, aching pain that develops after standing or sitting for long periods, as this allows pressure to build up in the enlarged veins. Activities that increase abdominal pressure, such as heavy lifting or strenuous exercise, can intensify the discomfort and, in some cases, may even contribute to the development of varicoceles. Painful varicoceles are often larger or more noticeable, though this is not always the case.
Fertility Problems
Varicoceles are often linked to infertility or reduced fertility, but determining whether they are the direct cause in a specific individual can be challenging. While many men with varicoceles father children without difficulty, the condition is believed to interfere with sperm production and quality in some cases. Factors such as the size of the varicocele, the duration it has been present, and individual health differences all play a role in whether fertility is affected. In one study, as many as 40% of men who were sub fertile were found to have a varicocele. Additional signs of varicoceles may include a reduced sperm count, poor sperm motility (movement), and a higher proportion of abnormally shaped sperm. The exact way varicoceles contribute to these issues is still uncertain, but one widely accepted theory suggests that the condition increases testicular temperature, which can interfere with healthy sperm production. Research indicates that 50–70% of men facing fertility challenges experience notable improvements in sperm quality and/or quantity following varicocele repair.
Testicular Atrophy
Testicular atrophy, or shrinkage, is another possible sign of a varicocele. The condition is frequently identified in teenage boys, often during routine sports physicals. If one testicle appears smaller than the other, treatment to repair the varicocele is usually advised. In many instances, the affected testicle regains its normal size after the procedure.
Diagnosis
- Physical Examination: In many cases, a varicocele can be identified during a routine physical check-up. Larger varicoceles may cause the scrotum to appear irregular or lumpy, often described as having a texture similar to a “bag of worms.”
- Doppler Ultrasound: If symptoms are less obvious, a colour flow Doppler ultrasound can be used. This painless and non-invasive imaging test helps detect abnormal blood flow patterns in the veins, making it easier to confirm the presence of a varicocele.
- Venogram: In some situations, a venogram may be performed. This involves injecting a contrast dye into the veins, followed by an X-ray, to clearly outline any irregularities in the blood vessels.
Note: In imaging studies, a prominent varicocele often shows up as visibly enlarged veins, consistent with the scrotum’s lumpy appearance.
Varicocele Treatment Options
In India, as well as globally, the conventional approach to managing varicoceles has typically been through open surgery, carried out by a urologist or a general surgeon. This method has been the standard for many years and involves making an incision to access and tie off the affected veins, thereby redirecting blood flow.
In more recent times, however, a minimally invasive option known as varicocele embolization has gained popularity. This procedure does not require open surgery, large incisions, or general anaesthesia. Instead, a small catheter is inserted into a vein, usually in the groin or neck, and guided to the affected area, where tiny coils or agents are placed to block the problematic veins. By sealing off these veins, blood is naturally rerouted through healthier pathways.
Because it is less painful, involves quicker recovery, and allows most patients to return to normal activities within a short period, varicocele embolization is increasingly becoming the preferred treatment choice for both doctors and patients.
Varicocele Surgery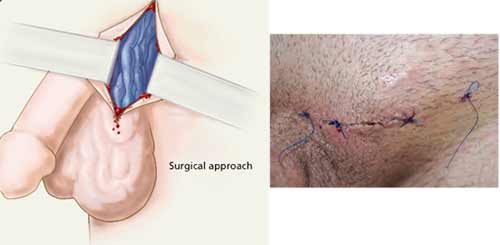
Varicocele Surgery is usually performed under general anaesthesia. Occasionally, the surgery is performed with a local anesthetic. During this procedure, the surgeon makes a small incision either just above the scrotum or higher up near the flank to access the affected area. The surrounding tissue layers are carefully opened to reach the dilated veins.
Once identified, the problematic veins are tied off (a process called ligation), which redirects blood flow into healthier veins. In certain situations, a laparoscope—a thin, tube-like instrument with a camera—is inserted into the abdomen to assist in performing the surgery with greater precision.
Recovery varies depending on the surgical approach, but most patients need several weeks before they can resume strenuous activities such as heavy lifting, with full recovery often taking up to six weeks.
Non-surgical – Varicocele Embolization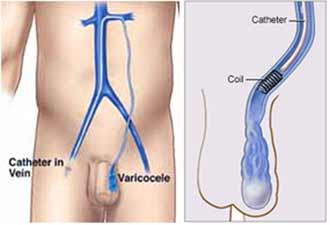
This non-surgical catheter directed embolization is an outpatient treatment. Specifically trained interventional radiologist makes a tiny nick in the skin at the groin or neck using local anesthesia and a thin catheter is passed and directed to the testicular vein. In varicocele embolization, an interventional radiologist begins by injecting a contrast dye, which helps create a detailed map of the veins and pinpoints the exact location of the problem. Through a thin catheter, small coils or embolic agents are then placed into the affected veins. These block abnormal blood flow and naturally redirect it into healthier venous pathways.
The procedure is minimally invasive, does not involve stitches, and typically lasts around 30 minutes. Once the catheter is removed, patients are kept under observation for a few hours before being discharged the same day. Recovery is usually very quick—most men feel little to no discomfort and are able to resume routine activities, including work, within 24 hours.
Beyond its convenience, varicocele embolization has been shown to be highly effective in improving male fertility. Research indicates that sperm concentration increases significantly in men undergoing this treatment, with about 83% showing improvement compared to 63% of those who underwent surgical ligation. Importantly, the overall cost of embolization is comparable to surgery, making it an equally accessible yet less invasive alternative.
Advantages of Varicocele Embolization
The majority of men in the INDIA undergo surgery as varicocele treatment. This is because they are usually sent to surgeons for evaluation, and many do not know about other treatment options available. So they agree for the surgery.
- Non surgical varicocele embolization is more effective than surgery, as measured by improvement in pain, semen analysis and pregnancy rates.
- It does not require any surgical incision in the scrotal area.
- A patient with varicoceles on both sides can have both fixed at the same time through one vein puncture site (surgery requires two separate open incisions)
- General anesthesia is not used for embolization (most surgery is done under general).
- There is a lower rate of complications compared to surgery. Infection has not been reported after embolization.
- It requires less recovery time. Post embolization patients are virtually never admitted to the hospital. Even patients with physically demanding jobs may return to work within the next day or two, unlike post surgical patients.