BACKACHE AND JOINTS PAIN
Back pain is very common. 8 out of every 10 people will have it at least once during their lives. Acute low back pain usually lasts for a few days to a few weeks and is caused by general work around the house or trauma from a sports or other injury. It can also be caused by arthritis. Acute back pain may vary from being a simple muscle ache to stabbing pain with decreased flexibility. Chronic back pain occurs when back pain lasts for 3 or more months.
Most people recover with treatment. At our department, we begin patients on conservative treatment including weight loss, medications and physiotherapy. If that fails, we consider interventions like minimally invasive Ozonucleolysis.
Slipped Disc
There are 24 bones called vertebrae in the cervical, thoracic and lumbar regions of the spine. Between each vertebra lies a soft, cushion-like disk that is filled with a gel-like substance. These intervertebral disks act as shock absorbers for the spine, allowing flexibility and smooth movement while also protecting the bones from grinding against one another. The jelly-like core, known as the nucleus pulposus, provides elasticity and resilience, while the tougher outer layer, the annulus fibrosus, holds everything in place and maintains spinal stability.
Sciatica
The sciatic nerve is a large nerve that goes from the lower back down each leg. It controls some muscles in the legs and sends feelings to the thigh, lower leg and foot. Sciatica is pain, weakness, numbness or tingling that can begin in the lower back and run down even to the toes. Usually, it affects one side of the body.
Symptoms of a slipped disc / Back pain
- The pain from a slipped disc can start in different ways. You might feel an ache in your lower back after you do something that you’re not used to. After a few hours, the pain can become so intense that moving around becomes very difficult.
- Or you may get severe pain all of a sudden, without warning. Some people say it can feel like being stabbed with a knife.
- Serious pain can stop you carrying out your normal activities.
Sciatica
- If you have a slipped disc in lumber region, you’ll almost always get pain in your buttocks, thighs, legs, and feet. Usually the pain is only on one side.
- You may also get numbness, weakness, or tingling in the same area.
- These symptoms mean the damaged disc is pressing on a sciatic nerve. These nerves run from the lower spine, passing through the buttocks and extending down the back of each leg all the way to the feet.
- Sciatica can come on at the same time as the back pain or it may come on later. The discomfort can radiate from the lower back down into the leg.
- With sciatica you can find it uncomfortable to sit down, stand up, or bend over. You will also find it painful to lift the affected leg while you’re lying down. This is one of the tests doctors use to diagnose sciatica.
- You can often get relief by getting into certain comfortable positions, such as lying down.
Other conditions that may cause Backache
Spondylitis and Ankylosing Spondylitis
Spondylitis is inflammation of the vertebrae that could be caused by genetic factors, an infection, chemicals or other agents. If the pain is confined to a particular nerve level, then treatment can be done.
Failed Back Syndrome
It is a chronic back or leg pain that happens after back surgery. Some causes of the syndrome include residual disk herniation, post-operative scar tissue, and pressure on a spinal nerve, altered joint mobility and muscular deconditioning.
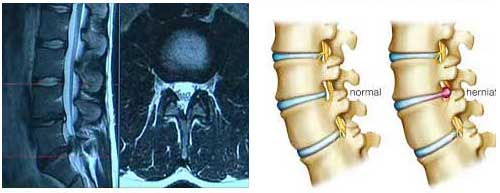
(A) MRI shows L5-S1 disc herniation (B) Normal spine and disc prolapsed spine
Arthritis

Osteoarthritis is inflammation of the joints that causes pain and swelling. An untreated swollen joint can lead to permanent damage. Osteoarthritis or degenerative joint disease can be caused by aging or repetitive injury and leads to damage of cartilage and bone. Arthritis may also be caused by the immune system attacking the body (autoimmune disease) such as in Rheumatoid arthritis.
Sports Injury
Some of the most frequent sports-related injuries are sprains, strains, knee problems, fractures, dislocations, Achilles tendon issues, muscle swelling, and pain along the shin bone.
Sprains and strains, which involve overstretching or tearing of ligaments and muscles, are generally minor and often begin to heal within 48 hours when managed with rest, application of ice or cold packs, and basic pain relief medication. However, more serious injuries such as fractures, dislocations, or tendon damage may require advanced medical care, including physiotherapy, immobilisation, or even surgery, depending on their severity. Early diagnosis and proper treatment are important to prevent long-term complications and to support safe return to physical activity.
Knee Pain.
The ligaments of the knee (MCL, ACL, and others) can be injured with trauma. .Menisci can be easily torn with sharp, rapid motions. The incidence of these tears increases with aging and degenerative conditions such as arthritis.
Tendinitis is inflammation of a knee tendon that can be caused by a strain such as jumping.
Frozen shoulder
A frozen shoulder is a stiff shoulder with low mobility and high pain. . 10 to 20% of patients with diabetes may experience a frozen shoulder.
Tennis/Golfer’s Elbow
Nowadays excessive computer use is more likely to cause tennis elbow than playing tennis. These conditions are sometimes caused by an injury.
Minimally Invasive Ozone Therapy for Disk Herniation
The appropriate treatment of lumbar sciatica, disk herniation and joint pain is a challenge. So many largely unknown or poorly understood factors are involved in the pathophysiology of these diseases that the right treatment is very difficult to pinpoint; this is the main reason so many treatments are continuously proposed.
Noninvasive procedures, minimally invasive percutaneous injection, and surgery represent the gamut of treatments available in the management of lumbar disk herniation. Noninvasive treatments are plainly the first choice in most cases, but when patients fail to respond, minimally invasive percutaneous injection or surgery is warranted. Many specialists are convinced that conservative treatment offers the same level of results, if checked at a late follow-up, as surgery. These approaches were specifically designed to achieve strong clinical outcomes while also being easier on the patient, both physically and financially.
Minimally invasive techniques generally involve smaller incisions, less trauma to surrounding tissues, and faster recovery times compared to conventional surgical methods. Because of their reduced complexity, they are often more cost-effective and better tolerated, allowing patients to return to daily activities much sooner. This combination of safety, efficiency, and affordability has made minimally invasive procedures a preferred choice in many areas of modern medicine. 5–20% treatment failure rate after surgical diskectomy , with failed back surgery syndrome in 15% of cases, further made minimally invasive procedures more popular.
Oxygen-ozone therapy is one of the most effective minimally invasive treatments currently available.
Actions of ozone are:
- Reduction in herniated disk volume, as disk shrinkage may reduce nerve root Compression.
- Disk shrinkage may also help to reduce venous stasis caused by disk compression of vessels, thereby improving local microcirculation and increasing the supply of oxygen. This effect has a positive effect on pain as the nerve roots are sensitive to hypoxia.
- Immunomodulating action
- Analgesic and anti-inflammatory effects
- Administering medical ozone followed by injection of a corticosteroid and an anesthetic at the same session gives better result.
Indications –
- Clinical signs of lumbar disk nerve root compression.
- CT and/or MR evidence of contained disk herniation.
- Chronic joint pain and swelling
Success rate: – 70-80%
Procedure –
Patient is given an intradiscal (4 mL) and periganglionic (8 mL) injection of an oxygen-ozone mixture at an appropriate concentration when ozone has a direct effect on the disk’s nucleus. The pulposus loses water molecules, leading to degeneration of its cellular matrix. Within about five weeks, this damaged tissue is gradually replaced by fibrous tissue, accompanied by the development of new blood vessels.Together, these events result in a reduction in disk volume thus relieving pain.
At the end of treatment, patients were advised to rest in supine decubitus position for 2 hours. Every patient was released from care on the same day the treatment was performed. All patients were able to return home on the day their treatment was carried out. Upon discharge, they were advised to slowly reintroduce physical activity rather than resuming full movement immediately. To monitor recovery and progress, follow-up evaluations were scheduled at three intervals—two weeks, two months, and six months after the procedure. The overall clinical results and effectiveness of the treatment were formally assessed at the six-month mark.
Complications — episodes of impaired sensitivity in the lower limb ipsilateral to the treatment; the episode resolved spontaneously within 2 hours.
Selection criteria for ozone therapy
The main clinical requirement for inclusion was the presence of persistent lower back pain that did not improve with standard conservative treatments such as medication, physiotherapy, or similar approaches. To qualify, the pain had to be ongoing for a minimum duration of three months despite these efforts, indicating a chronic and treatment-resistant condition.
Neurologic criterion was low back pain with positive signs of nerve root involvement, with or without paraesthesia or hypoesthesia, with appropriate dermatome distribution.
The neuroradiological criteria required confirmation through CT and/or MRI scans showing evidence of a contained disk herniation. These imaging findings needed to align with the patient’s clinical symptoms, ensuring that the radiologic results were consistent with the individual’s reported condition.
Residues of surgical micro diskectomy with recurrent herniation.
Exclusion criteria for oxygen-ozone therapy were: –
Neuroradiologic evidence of disk prolapse or free fragments of herniated disk, major neurologic deficit correlated to disk disease.
Non-surgical Minimally Invasive Interventional Procedure:
These procedures are performed without surgery by interventional radiologists. These physicians specialize in the use of X-rays, Digital subtraction angiography (DSA) and other techniques such as ultrasound, computed tomography (CT) and magnetic resonance (MR) to see inside the body without surgery. Slender, flexible tubes known as catheters are carefully inserted either through the skin or into blood vessels, depending on the procedure. Using imaging guidance, these catheters are then navigated through the body’s vascular pathways until they reach the exact area that requires treatment. This approach is similar to what is done during a heart angioplasty, where a catheter is guided to the coronary arteries to restore proper blood flow. The technique allows doctors to deliver treatment directly to the targeted site with precision, while avoiding the need for large incisions or open surgery.

As it is done by interventional Radiologist, he can see inside the body without opening it through CT scan, ultrasound, DSA thereby treating exact site of disease without effecting surrounding structures.
- It is less risky as compared to surgery
- It is cheaper than traditional surgery.
- No surgical scar on skin.
- Exact localization of the disease is possible through image guidance.
- Procedure done under local anesthesia.
- It is done as an outpatient (OPD) / day care or short hospital stay.
- Patients can resume normal activities within one to two day.
- It can fast relieve pain and suffering for many cancer patients
- Its safety has been proven over many years in thousands of people.
The pros and cons of the various techniques depend on the skill of the doctor performing the procedure and the availability of the necessary equipment. The patient should discuss the various procedures thoroughly with their primary physician and interventional radiologist.
Dr. Pradeep Muley is trained in the USA and Singapore and has performed over 20,000 non-surgical treatments for various diseases like uterine fibroids, uterine adenomyosis, un-operable liver tumor, liver abscesses, varicose vein, brain aneurysm and vomiting of blood from lungs and stomach. He runs the VARICOSE VEIN AND FIBROID CLINIC AT FORTIS HOSPITAL, VASANT KUNJ, NEW DELHI & created INDIA’S 1ST UTERINE FIBROID CLUB. He has treated the maximum number of fibroid patients in India through the innovative Uterine Artery Embolization method.
For more in-depth information on various non-surgical treatments available-
Mail Us: muleypradeep@hotmail.com or Visit to Website: – www.indianinterventionalradiology.com
Phone or Whatsapp: +91-9810492778
