Pelvic Congestion Syndrome (PCS)
Also called Painful Ovarian Varicose Veins and the very Effective Treatment is by technique called embolization
Chronic pelvic pain is a common condition and about 1/3 of all women experience this in their lifetime. Many women are often dismissed with the suggestion that their pain is “all in their head.” However, recent research indicates that the discomfort may actually be caused by varicose veins in the pelvis, which are difficult to detect and can lead to a condition known as pelvic congestion syndrome.
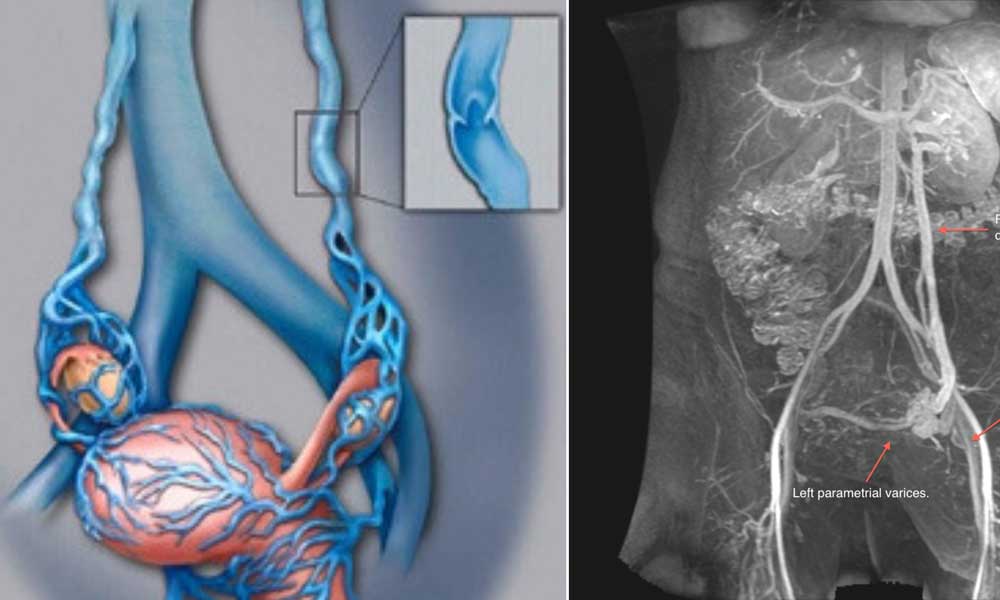
Faulty valves in the veins allow blood to accumulate, increasing pressure and causing the veins to bulge, which can result in pain. Pelvic congestion syndrome is often overlooked because during a pelvic exam, women lie down, which relieves pressure in the ovarian veins. As a result, the veins do not bulge with blood as they normally would when standing, making the condition harder to detect.
Living with chronic pelvic pain can be extremely challenging, impacting not just the woman experiencing it but also her relationships with family and friends, daily activities, and overall quality of life.
If your pelvic pain tends to worsen as the day goes on, especially when standing, it may be worth seeking a second opinion from an interventional radiologist. These specialists can collaborate with your gynecologist to evaluate and manage conditions like pelvic congestion syndrome. To explore this option, you can request a referral from your primary doctor, directly contact an interventional radiologist, or schedule a consultation online or by phone. Early assessment can help identify underlying causes and provide treatment options that improve comfort and daily functioning.
Prevalence and Symptoms
- Pelvic congestion syndrome typically affects women of childbearing age, usually under 45 years old.
- The commonest cause is previous pregnancy that causes incompetency of pelvic veins.
- The discomfort is often a dull, aching sensation located in the lower abdomen and lower back.
- The pain often increases during following intercourse, menstrual periods, when tired or when standing (worse at end of day).
Associated other symptoms include:
- Irritable bladder
- Abnormal menstrual bleeding
- Excessive Vaginal discharge
- Varicose veins on vulva, buttocks or thigh.
Diagnosis and Assessment
After excluding other causes such as structural abnormalities or inflammation through a detailed pelvic examination and ultrasound, pelvic congestion syndrome can be evaluated by an interventional radiologist—a physician specially trained in minimally invasive procedures guided by imaging techniques. To confirm the presence of pelvic varicose veins, the radiologist may recommend additional tests such as venography, CT or MRI venography, and Doppler ultrasound. These investigations help map the affected veins, assess blood flow, and determine the severity of the condition, providing precise information for planning targeted treatment.
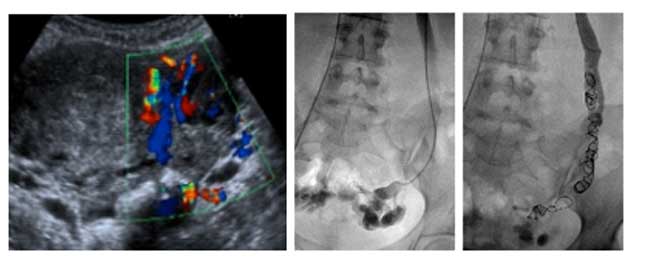
Pelvic Venography: Considered one of the most precise diagnostic tools for pelvic congestion syndrome, pelvic venography involves injecting a special contrast dye into the veins of the pelvic organs. This dye makes the veins clearly visible on X-ray imaging. During the procedure, dilated and varicose veins stand out prominently, allowing the interventional radiologist to identify abnormal blood flow, locate the affected veins, and plan targeted treatment. This technique provides detailed insight into the vascular anatomy of the pelvis, which is often difficult to assess with standard imaging alone.
Picture: – 1. USG Doppler study of pelvis shows prominent ovarian veins. |
MRI: Magnetic Resonance Imaging can be one of the most effective non-invasive methods for diagnosing pelvic congestion syndrome. However, the scan must be performed using a specialized protocol tailored to visualize the pelvic veins. A standard MRI often cannot detect the dilated or varicose veins associated with the condition, so the modified approach ensures clear imaging of blood flow and vascular abnormalities in the pelvis. This allows the interventional radiologist to accurately assess the extent of venous congestion without the need for invasive procedures.
Pelvic/ Transvaginal / Doppler Ultrasound: Usually not very helpful in diagnosing pelvic congestion syndrome unless done with the patient standing. Ultrasound can help rule out other conditions that may be contributing to pelvic pain.
Treatment Options
Once pelvic congestion syndrome is diagnosed and the patient is experiencing symptoms, embolization is recommended as a first-line treatment. Embolization is a minimally invasive, image-guided procedure performed by an interventional radiologist. During the procedure, a thin catheter is inserted through a small puncture in the groin and carefully navigated to the affected pelvic veins under X-ray guidance.
To relieve the painful pressure and correct the abnormal blood flow, the interventional radiologist places tiny coils, often combined with a sclerosing agent (similar to what is used to treat leg varicose veins), which effectively seals the enlarged veins. Because the procedure is minimally invasive, it is typically performed on an outpatient basis, allowing patients to return to normal activities immediately after treatment.
For cases where embolization is not suitable or has failed, surgical options may be considered. These include hysterectomy with removal of the ovaries, or ligation/removal of the affected veins, which are more invasive and require longer recovery times.
How effective embolization treatment
Embolization provides a safe, effective, and minimally invasive alternative to surgery that is also more cost-effective. The procedure reliably blocks the abnormal blood flow in the affected veins, helping patients return to normal activities with minimal recovery time.
Dr. Pradeep Muley is trained in the USA and Singapore and has performed over 20,000 non-surgical treatments for various diseases like uterine fibroids, uterine adenomyosis, un-operable liver tumor, liver abscesses, varicose vein, brain aneurysm and vomiting of blood from lungs and stomach. He runs the VARICOSE VEIN AND FIBROID CLINIC AT FORTIS HOSPITAL, VASANT KUNJ, NEW DELHI & created INDIA’S 1ST UTERINE FIBROID CLUB. He has treated the maximum number of fibroid patients in India through the innovative Uterine Artery Embolization method.
For more in-depth information on various non-surgical treatments available-
Mail Us: muleypradeep@hotmail.com or Visit to Website: – www.indianinterventionalradiology.com
Phone or Whatsapp: +91-9810492778