What is uterine / uterus fibroid ?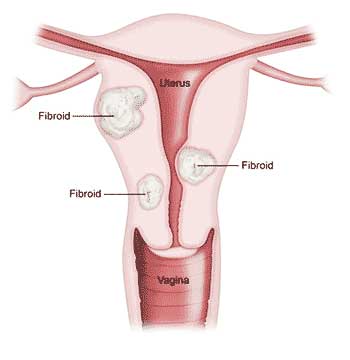
Uterine fibroids (myomas, leiomyomas, or fibromyomas) are the most frequent tumour found in the female reproductive system. Around 20 to 40% of women in their childbearing age have fibroids. Their size can vary from very small to as large as an orange or even bigger. In some cases, they may cause the uterus to enlarge, sometimes reaching the size of a pregnancy at about five months or more. Women between the ages of 30 and 50 are most prone to developing fibroids. Being overweight or obese further increases the likelihood of fibroids compared to women with a healthy body weight.
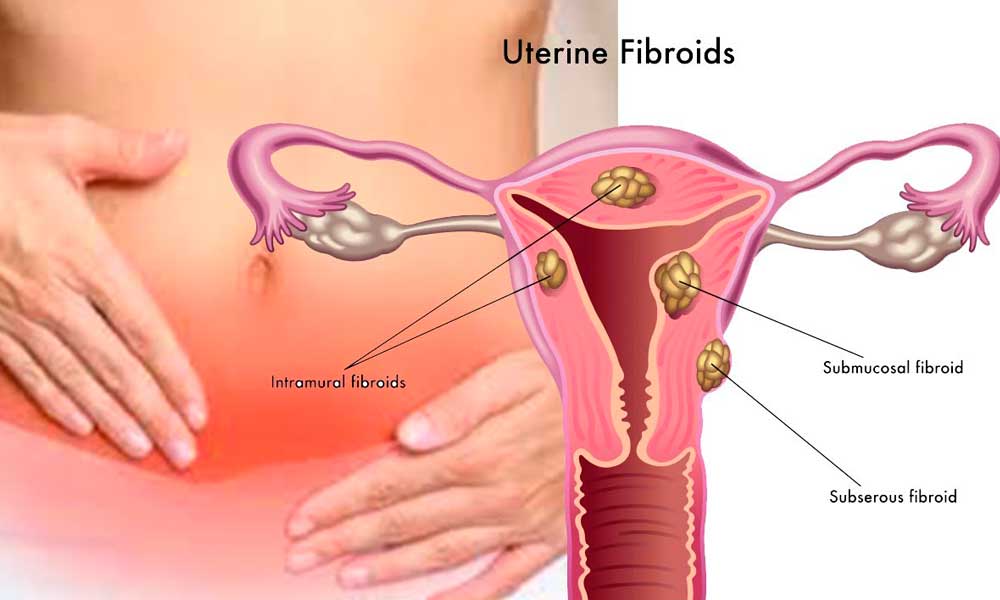
Types of uterine Fibroids
Fibroids are named according to their location within the uterus:
- Intramural fibroids grow within the wall of the uterus and are the most common type. Often, they cause no symptoms unless they become large. However, they can result in heavy bleeding with clots during the monthly cycle, and over time, may expand inward, leading to distortion and enlargement of the uterine cavity.
- Subserosal fibroids develop on the outer surface of the uterus and they grow vary large. Their size and location may exert pressure on adjacent organs such as the bladder and rectum, giving rise to symptoms like increased frequent or urgent urination, constipation, and lower back pain.
- Submucosal fibroids form within the muscle just below the uterine lining (endometrium), extending into the cavity of the uterus. Even small growths in this area can cause significant symptoms, including heavy bleeding and difficulties with fertility.
- Cervical fibroids arise in the wall of the cervix (the neck of the uterus). Depending on their size and location, they may block the cervical canal, causing infertility,pain, bleeding and problums during vaginal delivery.
Symptoms of fibroids:
- Heavy, prolonged menstrual periods and unusual bleeding with clots can lead to anaemia.
- Lower abdomen, back or leg pain
- Lower abdominal pressure or heaviness
- Bladder pressure leads to an urge to urinate.
- Pressure on bowel, leading to constipation and bloating
- Abnormally enlarged abdomen
Diagnosis
Fibroids are usually suspected during a routine gynaecological examination. An ultrasound scan of the lower abdomen is most commonly used to diagnose.. In addition, magnetic resonance imaging (MRI) can also provide a detailed diagnosis. Undergoing an MRI before beginning any treatment is generally recommended, as it helps to diagnose location and number of fibroids to plan line of treatment. These imaging tests also act as a reference point for follow-up evaluations after uterine fibroid embolization (UFE) or any other therapeutic procedure.
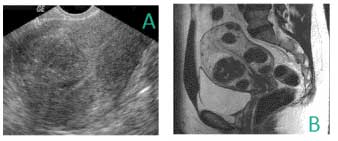
Picture A: Ultrasound image showing a submucosal fibroid.
Picture B: MRI image revealing multiple intramural fibroids.
Causes
The exact cause remains unclear; however, medical research and clinical findings suggest several contributing factors:
- Genetic changes: A large number of fibroids show genetic variations that differ from those seen in normal uterine muscle tissue.
- Hormonal influence: Oestrogen & progesterone, the two main hormones responsible for stimulating the uterine lining to prepare for pregnancy during each menstrual cycle, are believed to play a major role in fibroid growth. Compared to healthy uterine muscle cells, fibroids contain a higher concentration of receptors for these hormones.
- Chemical factors: Certain substances that regulate and support tissue maintenance in the body, such as insulin-like growth factors, may also have an impact on the development and growth of fibroids.
Complications
Although uterine fibroids are not dangerous, they can cause discomfort and may lead to complications such as anemia from heavy bleeding or large fibroids.
- Anaemia: if bleeding is heavy caused by fibroids can result in anaemia, leaving the individual weak, fatigued, and prone to other health issues.
- Urinary tract infections: When fibroids put pressure on the urinary bladder and prevent it from emptying completely, the risk of recurrent urinary tract infections increases.
- Fibroids and pregnancy: In most cases, fibroids do not interfere with fertility or a healthy pregnancy. However, there are instances where fibroids may distort or obstruct the fallopian tubes, hindering the movement of sperm from the cervix to the tubes, thereby affecting conception. Treatment for fibroids during pregnancy is often not required, but a frequent complication is localised pain, particularly between the first and second trimesters, which can usually be managed with standard pain relief. In some situations, fibroids may be linked to repeated pregnancy losses, especially when no other identifiable cause of miscarriage is found.
Treatment Options for Fibroids
There is no single best method for treating uterine fibroids, as multiple treatment options are available depending on the severity of the condition and the individual’s needs.
- Observation (Watchful waiting): A large number of women with fibroids do not show any symptoms. In such cases, careful monitoring or expectant management may be the most suitable approach. Since fibroids are non-cancerous, immediate treatment is not always necessary.
- Medication: Certain medicines can help in managing and easing mild symptoms associated with fibroids, such as pain or heavy bleeding. However, these drugs do not eliminate or cure the fibroids themselves; they only provide temporary relief.
- Non-surgical: – A. Uterine artery embolization. B. HIFU
- Surgical: – A. Hysterectomy B. Myomectomy
Medications
Medications for uterine fibroids work by targeting the hormones that control your menstrual cycle, helping to relieve symptoms like heavy bleeding and pelvic pressure. However, they do not shrink or completely remove fibroids. Common options include::
- (GnRH) Agonists-Releasing Hormone: Drugs known as GnRH agonists are sometimes prescribed for fibroid management. They work by lowering the body’s natural oestrogen and progesterone levels, creating a temporary state similar to menopause. While effective in shrinking fibroids and easing symptoms, many women experience noticeable side effects during treatment, the most common being frequent and intense hot flashes.
- Androgens: This medication, similar to male hormone testosterone, can temporarily stop menstruation and help correct symptoms. While it can be effective, it is rarely prescribed for fibroid treatment. Many women avoid its use because of potential side effects such as weight gain, acne, headaches, unwanted hair growth, mood disturbances like depression or anxiety, and, in some cases, a deepening of the voice.
Non – Surgical Treatment options for uterine fibroids
A.Uterine artery embolization / Uterine Fibroid embolization:
It is a minimally invasive interventional radiological procedure, which means it requires only a tiny nick in the skin. It is performed under reginoal anesthesia – feeling no pain and usually requires a hospital stay of one night. Most women after treatment can resume normal activities within a few days and majority of women are able to return to their regular activity within a week.
UFE treats all uterine fibroids at the same time and is, therefore, extremely effective.
Ideal Patient for uterine fibroid embolization
- They have single or multiple fibroids
- The fibroids are symptomatic
- There is no cancer
- A desire to retain her uterus.
- Does not desire surgery.
- Poor surgical candidate (e.g., because of obesity, bleeding disorders, anemia).
The interventional Radiologist makes a small nick in the skin (less the ¼ of an inch) at groin, inserts a catheter, identifies uterine artery by using angiography with contrast media injection and then inject embolization particles (polyvinyl alcohol) that block the tiny vessels supplying all the fibroids. This blockade of blood supply to fibroids causes infarction (loss of blood supply to the fibroids) and subsequent degeneration of the fibroids and it starts reducing in size reaching half the size in few weeks. Symptoms due to the fibroids (like bleeding and pain) resolve in 85% to 95% of patients.
Uterine Artery Embolization has many Indications:-
- Single / multiple Uterine Fibroids.
- Adenomyosis.
- Failed myomectomy / recurrence of fibroids after myomectomy
- High risk patient for surgery like obesity, anemia, Chronic renal failure etc.
- Post-partum Hemorrhage
- Bleeding from Cancer of Cervix & Uterus
- Pre-operative embolization to reduce bleeding during uterine surgery.
Side effects:
- About 1% chance for infection which is typically characterized by fever and smell from vagina. It just needs antibiotics to treat.
- Mild pelvic pain will remain for 1-2 days and it is controlled very well by simple pain medication.
- Mild fever which is well controlled by paracetamol oral tablets.
- About a half percentage of the woman land-up in short term menopause. Later they may resume normal periods.
- Women those have fibroids always have risk of fertility. Despite these risks, many women have had successful pregnancies following uterine artery embolization
Pros & Cons of non-surgical treatment: It shows overall success rate of about 96-98% which is unlikely in other methods of fibroid treatment.
- It is the only method that can treat multiple fibroids in one sitting.
- Uterine artery embolization treats the fibroids and adenomyosis together.
- No surgical scar or blood loss during the procedure.
- It needs just daycare or 24 hrs hospitalization.
- Short recovery time just 1-4 Days.
Advantages of Uterine artery embolization
- It is performed under Local anesthesia. Not General anesthesia.
- Requires only a tiny nick in the skin (No surgical incision of abdomen).
- Recovery is shorter than from hysterectomy or open myomectomy.
- Virtually no adhesion formation has been found. But in surgery adhesions are common.
- All fibroids are treated at once, which is not the case with myomectomy.
- Recurrent growth of treated fibroids is uncommon.
- The procedure is associated with minimal blood loss, virtually eliminating the need for a blood transfusion.
- For women whose primary symptom was heavy vaginal bleeding, 87–98% report significant improvement or complete resolution of bleeding within just 24 hours after the procedure.
- Emotionally, financially and physically – embolization can have an overall advantage over other procedures for the patient as the uterus is not removed.
B. Focused ultrasound surgery: –
MRI-guided focused ultrasound surgery (FUS) is a noninvasive procedure that targets and treats uterine fibroids without removing the uterus. This procedure is performed while you’re inside of a specially crafted MRI scanner that allows doctors to visualize your anatomy, and then locate and destroy (ablate) fibroids inside your uterus without making an incision. Focused high-frequency, high-energy sound waves are used to target and destroy the fibroids. One or two treatment sessions are done in an on- and off-again fashion, sometimes spanning several hours.
Since FUS is a new technology, researchers are learning more about the long- term safety and effectiveness of FUS.
Surgical Treatment options for uterine fibroids
A. Hysterectomy (removal of uterus)
What it is:
Hysterectomy is the surgical removal of the uterus, typically carried out by a gynaecologist. Hysterectomy may be total (removing complete uterus including cervix) or partial (removal of the uterus leaving the cervix intact). Ovaries may also be removed at the same time.
How it is done it is a major surgery and needs general anesthesia. It requires a surgical cut, the size of the scar depends on how big the uterus is. It can be abdominal, vaginal or laparoscopic.
Side effects
Risk of bleeding, which may sometimes necessitate a blood transfusion.
Long term morbidity is relatively more under the age of 45 years believed to be caused by the hormonal side effects of hysterectomy and prophylactic oophorectomy.
Approximately 35% of women after hysterectomy undergo another related surgery within 2 years.
Ureteral(Urinary Tube) injury is not uncommon and can range from 2.2% to 3%.
Pros & Cons of surgery – Hospital stay is 2 to 5 days or more. Time for full recovery is very long in all types of hysterectomy whether abdominal, vaginal or laparoscopic. Definition of “full recovery” means 3 to 12 months. Serious limitations in everyday activities are expected for a minimum of 4 months.
It permanently ends your ability to have children, and if the ovaries are also removed, it induces menopause, raising the consideration of whether hormone replacement therapy will be needed.
B.Myomectomy (removal of fibroid)
What it is: It is surgical removal of the fibroids, usually performed by a gynecologist. Myomectomy may be open or by laparoscopic approach. Sometimes it is done by hysteroscope. Whatever is the approach it is a major surgery.
How it is done. It needs general anesthesia and requires surgical cut in lower abdomen, the size of the scar depends on how big the fibroid is. It can be abdominal or laparoscopic.
Side effects Excessive blood loss. The uterus is richly supplied with blood vessels, and fibroids encourage the formation of new vessels to secure their own blood supply. Therefore, during a myomectomy, surgeons must take special precautions to minimise the risk of excessive bleeding.
Scar tissue. Incisions into the uterus to remove fibroids can lead to adhesions — bands of scar tissue that may develop after surgery. Within the uterus, adhesions may block implantation of a fertilized egg in the uterine lining and adhesions could entangle neighboring structures and lead to a blocked fallopian tube or a trapped loop of intestine.
Development of new fibroids. Myomectomy doesn’t eliminate your risk of developing more fibroids later. Instead, the very small invisible fibroid start growing at a much faster rate leading to a high rate of recurrence. If fibroids return, future treatment — a repeat myomectomy, hysterectomy or other procedure — may be necessary.
Childbirth complications. If myomectomy incision is deep it may weaken the uterine wall which may pose problem in future childbirth. Your gynecologist may recommend cesarean delivery to avoid rupture of the uterus during labor.
Pros & Cons of surgery – Hospital stay is 2 to 5 days or more. Time for full recovery is very long ie few months.
Best solution for fibroid treatment – Non surgical treatment Uterine artery embolization
Uterine artery embolization (UAE) is a procedure where an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the fibroids. When performed specifically to treat uterine fibroids, the procedure is referred to as uterine fibroid embolization (UFE). The procedure is not a surgical intervention and allows the uterus to be kept in place, relieving the patient of its symptoms with quick recovery and quick resumption of day to day activities.
Benefits of non-surgical treatment
- It is performed under Local anesthesia. Not General anesthesia.
- Requires only a tiny nick in the skin (No surgical incision of abdomen).
- Recovery is shorter than from hysterectomy or open myomectomy.
- Virtually no adhesion formation has been found. But in surgery adhesions are common.
- Unlike myomectomy, uterine fibroid embolization treats all fibroids in a single procedure.
- Recurrent growth of treated fibroids is uncommon.
- Uterine fibroid embolization is associated with minimal blood loss and carries almost no risk of requiring a blood transfusion.
- For women whose primary symptom was heavy vaginal bleeding, 87–90% experience significant improvement or complete resolution within just 24 hours.
- Emotionally, financially and physically – embolization can have an overall advantage over other procedures for the patient as the uterus is not removed.